Patella Dislocation Treatment
Description:
Patella dislocation, also known as kneecap dislocation, is a medical condition where the patella (kneecap) moves out of its normal position within the patellofemoral groove in the femur towards the outside onto the femoral condyle (thigh bone). This mostly occurs as a disruption of the medial patellofemoral ligament amd can result in pain, instability, and limited knee function. To effectively manage patella dislocation, it's crucial to understand its causes, symptoms, and potential risks.
Acute patella dislocation can either be traumatic or atraumatic:
o Traumatic: good history of trauma and development of swelling within the joint post injury.
o Atraumatic: usually occurs in females with associated ligament laxity, no history of trauma, accompanied by mild-to-moderate swelling.
- The incidence of acute patella dislocation is 2-3%.
- Patella dislocations are most common in females in the second decade of life.
- The main differential diagnosis is an ACL rupture as both condition present very similarly.
Presentation
- Mechanism of injury:
o Atraumatic: a twisting or jumping movement that results in the knee suddenly giving way with the development of severe pain.
o Traumatic: a direct blow to the knee.
- People may describe a ‘popping out’ feeling.
- Instability of the knee post incident.
- Immediate swelling.
- Straightening of the knee usually reduced the dislocation spontaneously, however, in some cases it may require some assistance.
- There is usually marked tenderness over the inside border of the kneecap.
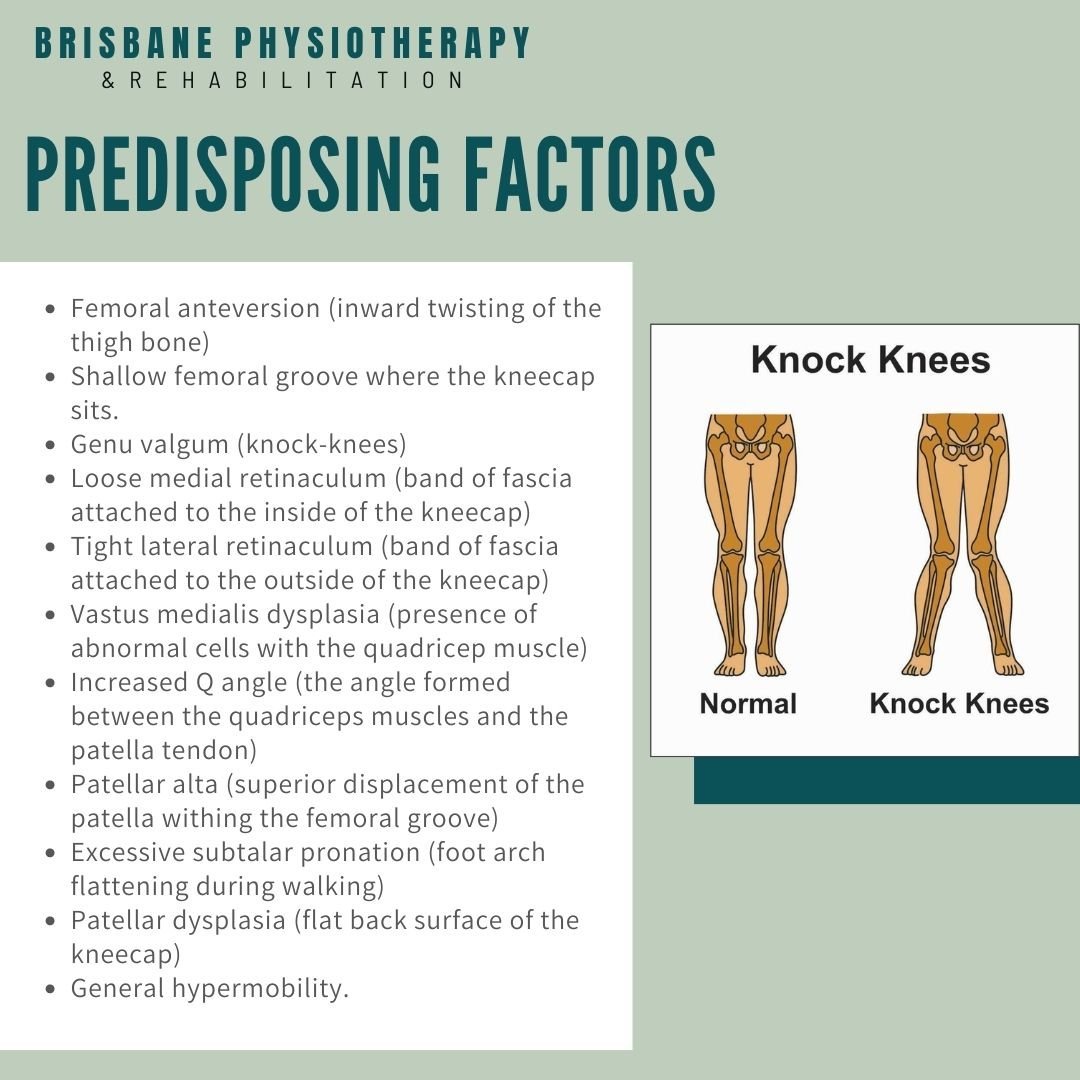
Predisposing Factors
- Femoral anteversion (inward twisting of the thigh bone)
- Shallow femoral groove where the kneecap sits.
- Genu valgum (knock-knees)
- Loose medial retinaculum (band of fascia attached to the inside of the kneecap)
- Tight lateral retinaculum (band of fascia attached to the outside of the kneecap)
- Vastus medialis dysplasia (presence of abnormal cells with the quadricep muscle)
- Increased Q angle (the angle formed between the quadriceps muscles and the patella tendon)
- Patellar alta (superior displacement of the patella withing the femoral groove)
- Excessive subtalar pronation (foot arch flattening during walking)
- Patellar dysplasia (flat back surface of the kneecap)
- General hypermobility.
Causes and Mechanisms:
Patella dislocation typically occurs due to:
Direct Trauma: A direct blow to the knee, often during sports or accidents, can dislocate the patella.
Muscular Imbalance: Muscle imbalances around the knee, particularly weak or tight muscles, can affect patellar alignment.
Structural Factors: Certain anatomical factors, such as a shallow patellofemoral groove or abnormalities in the patellar shape, can predispose individuals to dislocations.
Signs and Symptoms:
Common signs and symptoms of patella dislocation include:
Knee Pain: Sudden and severe pain in the knee, particularly after a traumatic event.
Swelling: The knee may swell due to inflammation and bleeding.
Visible Dislocation: In some cases, the dislocated patella can be visibly displaced, creating an abnormal knee shape.
Instability: A sense of knee instability, making it difficult to bear weight on the affected leg.
Limited Range of Motion: Difficulty in bending or straightening the knee.
Management Strategies:
Reduction:
The first step in managing a patella dislocation is to have a healthcare provider gently reposition the patella back into its normal location. This process is called reduction and should only be performed by a medical professional.
Immobilization:
After reduction, the knee may be immobilized with a brace or cast to prevent further dislocation and allow the joint to heal. It's essential to follow your healthcare provider's instructions on brace usage.
Physical Therapy:
Physical therapy is a key component of rehabilitation. A physical therapist will design a program to improve muscle strength, balance, and joint stability in the knee. Specific exercises will target the quadriceps and hamstrings, which play a critical role in kneecap stability.
Surgical Intervention:
In some cases, especially when there are recurrent dislocations, significant damage, or anatomical issues, surgical procedures may be necessary. Surgical options include realigning the patella, stabilizing it, or addressing structural factors contributing to dislocation.
Bracing and Support:
Your healthcare provider may recommend a knee brace or support to enhance stability and prevent recurrence. These braces are designed to keep the patella aligned.
Pain Management:
Over-the-counter pain relievers, prescribed medications, or physical modalities like ice and heat can help manage pain and inflammation. Always follow recommended dosages and consult with a healthcare provider.
Rehabilitation and Preventive Measures:
Continue with the prescribed physical therapy program even after initial recovery. Building strength and stability in the knee is essential to prevent future dislocations.
Maintain a healthy lifestyle, including a balanced diet and regular exercise to support overall knee health.
Wear protective gear, such as knee braces, during high-risk activities or sports.
Pay attention to your body and be cautious when engaging in physical activities. Promptly address any discomfort or concerns.
Kneecap Dislocation Treatment
Atraumatic dislocations are treated conservatively.
Traumatic first or second-time dislocations with knee joint swelling are treated with arthroscopic washout and debridement.
Recurrent dislocations are treated with surgical stabilization.
Aim of rehabilitation: reduce injury reoccurrence. As a result, rehabilitation is lengthy and emphasizes on core stability, pelvic positioning, quadricep strengthening and stretching of the lateral structures.
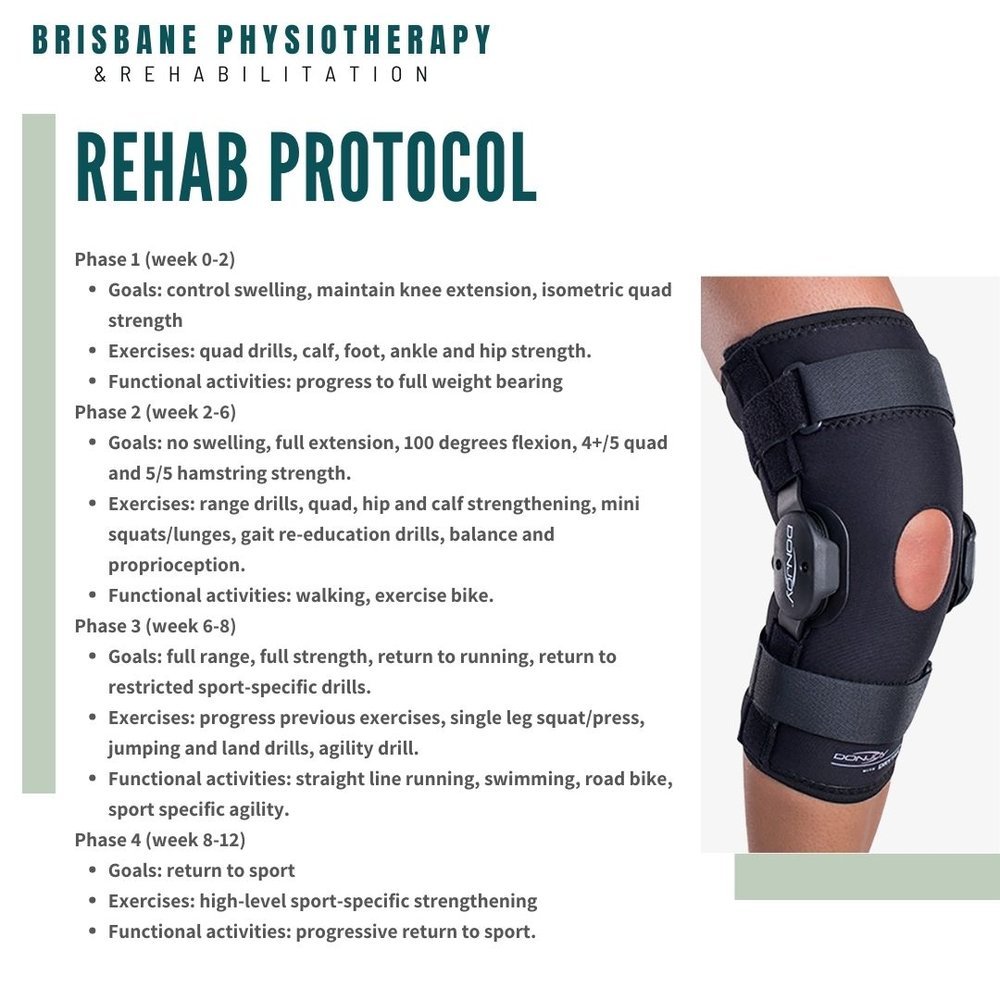
Rehabilitation protocol.
- Phase 1 (week 0-2)
o Goals: control swelling, maintain knee extension, isometric quad strength
o Physio: extension splint, cryotherapy, electrotherapy, taping, manual therapy.
o Exercises: quad drills, calf, foot, ankle and hip strength.
o Functional activities: progress to full weight bearing
- Phase 2 (week 2-6)
o Goals: no swelling, full extension, 100 degrees flexion, 4+/5 quad and 5/5 hamstring strength.
o Physio: cryotherapy, electrotherapy, compression, manual therapy, gair-re-education, exercise modification.
o Exercises: range drills, quad, hip and calf strengthening, mini squats/lunges, gait re-education drills, balance and proprioception.
o Functional activities: walking, exercise bike.
- Phase 3 (week 6-8)
o Goals: full range, full strength, return to running, return to restricted sport-specific drills.
o Physio: manual therapy, exercise/activity modification.
o Exercises: progress previous exercises, single leg squat/press, jumping and land drills, agility drill.
o Functional activities: straight line running, swimming, road bike, sport specific agility.
- Phase 4 (week 8-12)
o Goals: return to sport
o Exercises: high-level sport-specific strengthening
o Functional activities: progressive return to sport.
Prognosis: patella dislocation rehabilitation usually takes around 8-12 weeks to return to sport.