Patella Fractures
What is a Patella Fracture?
A patella fracture involves a break or crack in the kneecap, which is a small, flat, triangular bone at the front of the knee. This type of fracture can occur due to various reasons, such as falls, direct trauma, or high-impact sports injuries. A comprehensive understanding of patella fractures, including their causes, symptoms, and management, is essential for effective treatment and recovery.
Patella Fracture Causes and Mechanisms:
Patella fractures can result from:
Direct Trauma: A direct blow to the knee, often occurring in falls or automobile accidents.
Sports Injuries: High-impact sports or activities that involve a risk of knee injuries may lead to patella fractures.
Risk Factors:
Certain factors may increase the risk of sustaining a patella fracture, including:
Participation in Sports: Engaging in activities with a risk of knee injuries.
Age: Older adults may be more prone to fractures due to changes in bone density.
Signs and Symptoms of a Patella Fracture:
Common signs and symptoms of a patella fracture include:
Pain: Immediate pain at the front of the knee.
Swelling: Swelling and tenderness around the fractured area.
Difficulty Straightening the Knee: Difficulty in extending or straightening the knee.
Bruising: Discoloration of the skin around the knee.
Patella Fracture Management Strategies:
Early Assessment:
A thorough assessment by a physiotherapist is essential to evaluate the extent of the patella fracture, assess surrounding structures, and identify individualized treatment needs.
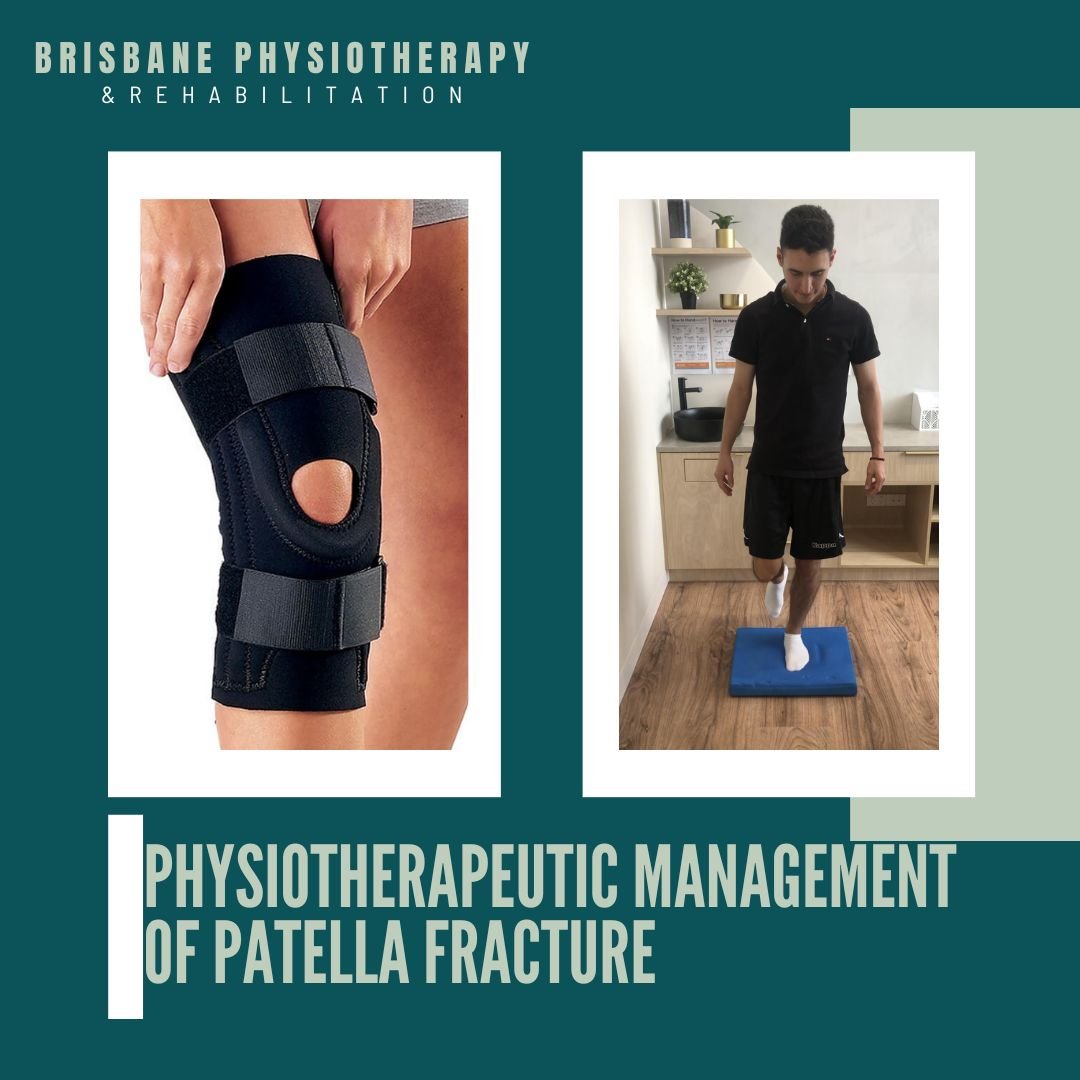
Immobilization Support:
Physiotherapists work with patients to adapt to braces, casts, or splints, ensuring they provide optimal support without hindering other aspects of daily life.
Pain Management:
Modalities such as heat or cold therapy, gentle massage, and specific exercises help manage pain and discomfort associated with the fracture.
Range of Motion Exercises:
Gradual introduction of passive and active range of motion exercises helps restore flexibility in the knee joint. This is initiated as early as possible, considering the stage of healing.
Strengthening Exercises:
Specific exercises targeting the muscles around the knee are introduced to rebuild strength gradually. Progressive resistance exercises ensure a safe and effective recovery.
Weight-Bearing Activities:
Physiotherapists guide patients through a gradual return to weight-bearing activities to prevent complications and promote recovery. This may involve exercises like partial weight-bearing or assisted walking.
Functional Activities:
Physiotherapists incorporate functional activities into rehabilitation, mimicking daily tasks to enhance coordination and promote the integration of the knee into regular movements.
Home Exercise Program:
Physiotherapists design personalized home exercise programs, emphasizing the importance of consistency to optimize recovery.
Patients are educated on self-management techniques and advised on when to seek professional guidance.
Gradual Return to Activities:
Physiotherapists work with patients to ensure a safe and gradual return to daily activities, including work and recreational pursuits.
Preventing Recurrence:
Education on injury prevention strategies, proper warm-up techniques, and ongoing exercises to maintain knee strength and flexibility are integral to preventing future injuries.
Patella Fracture ORIF
What is a Patella Fracture ORIF?
A patella fracture ORIF (Open Reduction Internal Fixation) is a surgical procedure performed to repair a broken patella, or kneecap, using metal screws, wires, or plates to hold the fractured bone fragments in place while they heal. The patella is a small, triangular bone located at the front of the knee joint, and fractures can occur due to direct trauma, such as a fall onto the knee or a sudden blow to the kneecap.
Patella fractures can vary in severity, from small cracks to complete breaks that result in displacement of the bone fragments. Indications for patella fracture ORIF include displaced fractures, fractures with multiple fragments, fractures that involve the joint surface, and fractures that impair knee function or stability.
Physiotherapy Management
Physiotherapy plays a crucial role in the rehabilitation process following patella fracture ORIF. The physiotherapist's goals are to promote healing, restore range of motion, regain strength and function, and facilitate the patient's return to normal activities.
In the early stages of rehabilitation, physiotherapy focuses on pain management and protecting the surgical site while allowing the fracture to heal. This may involve the use of assistive devices such as crutches and wearing of a knee braces to limit weight-bearing on the affected leg and prevent excessive stress on the healing bone.
Range of motion exercises are initiated early to prevent stiffness and improve flexibility in the knee joint. These exercises may include gentle knee bends, straight leg raises, and passive stretching techniques performed under the guidance of the physiotherapist.
As healing progresses, the physiotherapy program is advanced to include strengthening exercises targeting the quadriceps, hamstrings, and calf muscles. These exercises help stabilise the knee joint and improve functional strength to support activities such as walking, climbing stairs, and rising from a seated position.
Physiotherapists also provide guidance on proper gait mechanics, weight-bearing progression, and activity modification to prevent complications and optimise long-term outcomes. Soft tissue massage, joint mobilisations, and proprioceptive training are often completed to address any residual stiffness, muscle imbalances, or proprioceptive deficits.
Conclusion
By following a comprehensive physiotherapy program, patients can achieve optimal outcomes, regain function, and return to their desired level of activity following patella fracture ORIF.