What is Quadriceps Tendinopathy?
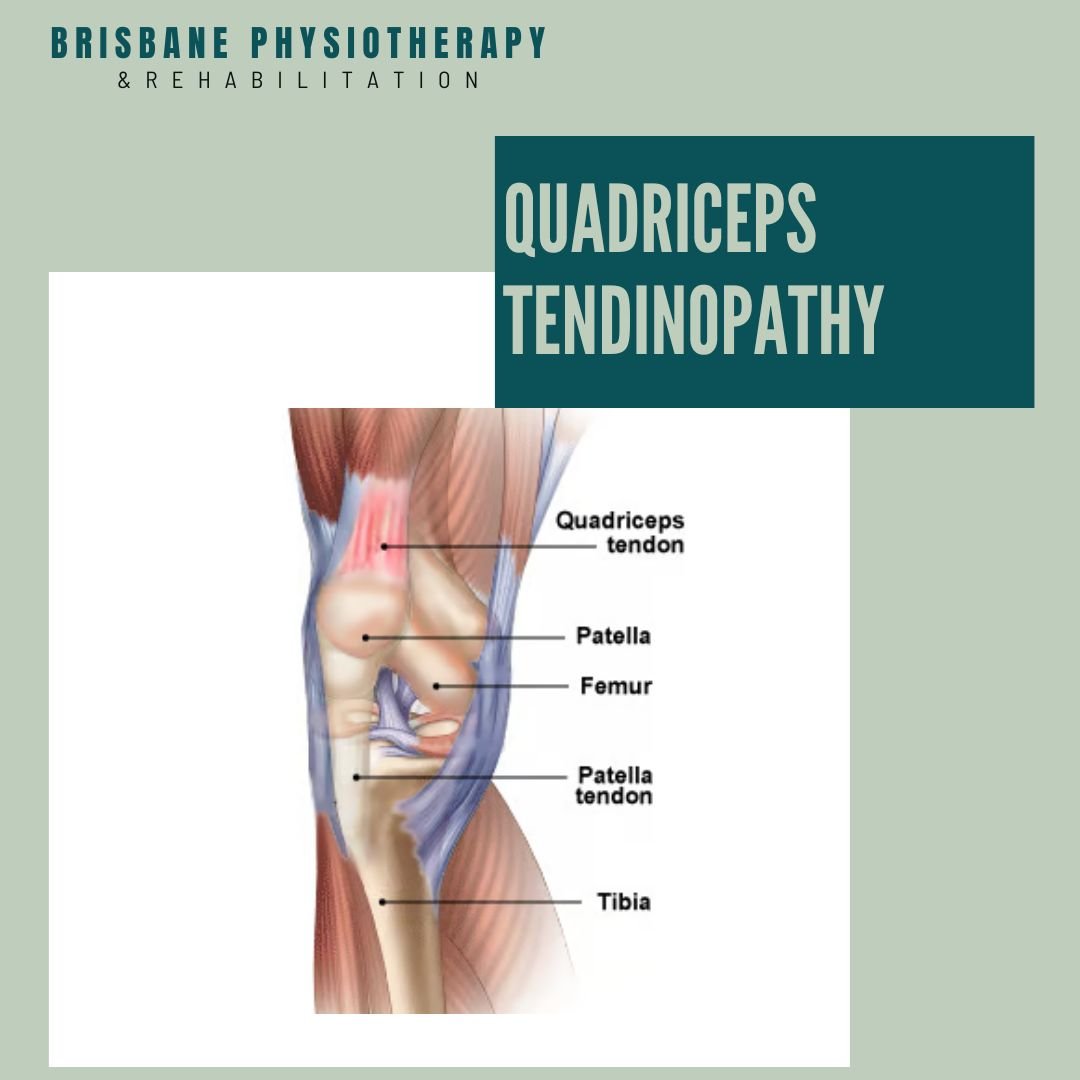
Quadriceps tendinopathy, refers to a condition characterised by degeneration, inflammation, or irritation of the quadriceps tendon. The quadriceps tendon is a thick, strong tendon that connects the quadriceps muscles to the patella (kneecap) and helps in knee extension.
Symptoms:
Pain: Pain is typically felt at the front of the knee, just above the patella. It may be described as a dull ache or sharp pain, especially during activities that involve jumping, running, or squatting.
Stiffness: Stiffness in the knee joint, particularly after periods of inactivity or prolonged sitting.
Tenderness: The area around the quadriceps tendon may be tender to the touch.
Swelling: Swelling or inflammation may occur around the affected tendon.
Weakness: Weakness or difficulty performing activities that require knee extension, such as climbing stairs or rising from a seated position.
Causes:
Overuse: Repetitive stress or overuse of the quadriceps tendon, especially in activities that involve running, jumping, or squatting, can lead to tendinopathy.
Poor Biomechanics: Abnormalities in lower limb alignment or mechanics, such as flat feet, leg length discrepancies, or muscle imbalances, can increase the risk of developing tendinopathy.
Training Errors: Rapidly increasing the intensity, duration, or frequency of physical activity without proper conditioning or rest can contribute to tendon overloading and injury.
Age: Tendinopathy is more common in middle-aged and older individuals due to age-related changes in tendon structure and function.
Previous Injury: A history of quadriceps tendon injuries or repetitive microtrauma can weaken the tendon and predispose it to degeneration and injury.
Treatment of Quadriceps Tendinopathy
The treatment of quadriceps tendinopathy typically involves a phased approach that focuses on reducing pain and inflammation, restoring strength and flexibility, correcting biomechanical abnormalities, and gradually returning to normal activities. Physiotherapy plays a crucial role in each stage of rehabilitation. Here's a general outline of the treatment stages with physiotherapy:
Stage 1: Pain Management and Protection
Goal: Reduce pain and inflammation, protect the injured tendon.
Physiotherapy Interventions:
Education: Understanding the condition, activity modification, and the importance of rest.
Ice Therapy: Applying ice packs to the affected area to reduce pain and inflammation.
Soft Tissue Mobilisation: Gentle massage techniques to relieve tension and improve blood flow.
Joint Mobilisation: Manual therapy techniques to improve joint mobility and reduce stiffness.
Taping or Bracing: Applying tape or using a brace to provide support and reduce stress on the tendon.
Isometric Exercises: Gentle contractions of the quadriceps muscles to maintain strength without aggravating the tendon.
Stage 2: Restoring Mobility and Flexibility
Goal: Improve range of motion, reduce stiffness, and restore normal biomechanics.
Physiotherapy Interventions:
Stretching Exercises: Gentle stretching of the quadriceps muscles and surrounding structures to improve flexibility.
Eccentric Strengthening: Gradual introduction of eccentric exercises to strengthen the quadriceps tendon while lengthening it, promoting tendon remodeling.
Manual Therapy: Continued soft tissue mobilisation and joint mobilisation to address any remaining stiffness.
Proprioceptive Training: Balance and proprioception exercises to improve joint stability and control.
Functional Activities: Incorporating functional movements that mimic daily activities to improve mobility and movement patterns.
Stage 3: Strengthening and Neuromuscular Control
Goal: Build strength in the quadriceps muscles, improve neuromuscular control, and enhance functional performance.
Physiotherapy Interventions:
Progressive Strengthening: Gradually increasing the intensity of exercises targeting the quadriceps muscles, including concentric, eccentric, and isometric exercises.
Plyometric Exercises: Controlled jumping and landing exercises to improve power and dynamic stability.
Agility and Coordination Training: Incorporating drills and exercises to improve coordination, agility, and movement efficiency.
Gait Training: Analysing and correcting walking or running patterns to reduce stress on the tendon.
Sport-Specific Training: Functional exercises tailored to the individual's specific sport or activities to prepare for a return to sport.
Stage 4: Return to Activity and Prevention
Goal: Gradually reintroduce sport-specific activities, prevent recurrence of injury.
Physiotherapy Interventions:
Gradual Return to Sport: Incrementally increasing the intensity and duration of activities, closely monitoring for any signs of pain or dysfunction.
Performance Enhancement: Addressing any remaining deficits in strength, flexibility, or biomechanics to optimise performance and reduce the risk of future injury.
Injury Prevention Program: Implementing a comprehensive program focusing on strength, flexibility, proprioception, and technique to reduce the risk of recurrence.
Throughout all stages of rehabilitation, your physiotherapist will closely monitor progress, modify the treatment plan as needed, and provide guidance and support to facilitate optimal recovery. It's essential to adhere to the prescribed exercises and recommendations to achieve the best outcomes and prevent further injury.