Total Hip Replacement
What is a Total Hip Replacement (THR)?
Overview of Total Hip Replacements:
- Total Hip Replacements are performed for people who have severe osteoarthritis that is making daily activities difficult and is no longer responding to other treatments.
- A Total Hip Replacement involves the surgical removal and replacement of the damaged femoral head and acetabulum of the hip joint with a prosthetic implant.
- Total Hip Replacements can be performed through different surgical approaches (anterior or posterior) based on the decision of the Orthopaedic Surgeon.
- Depending on the type of surgical approach, different wound areas and post-operative precautions will apply.
- All joint replacements are major, planned 1–2-hour surgeries requiring admission to hospital, anaesthesia and post-operative hospital recovery.
Hip Precautions
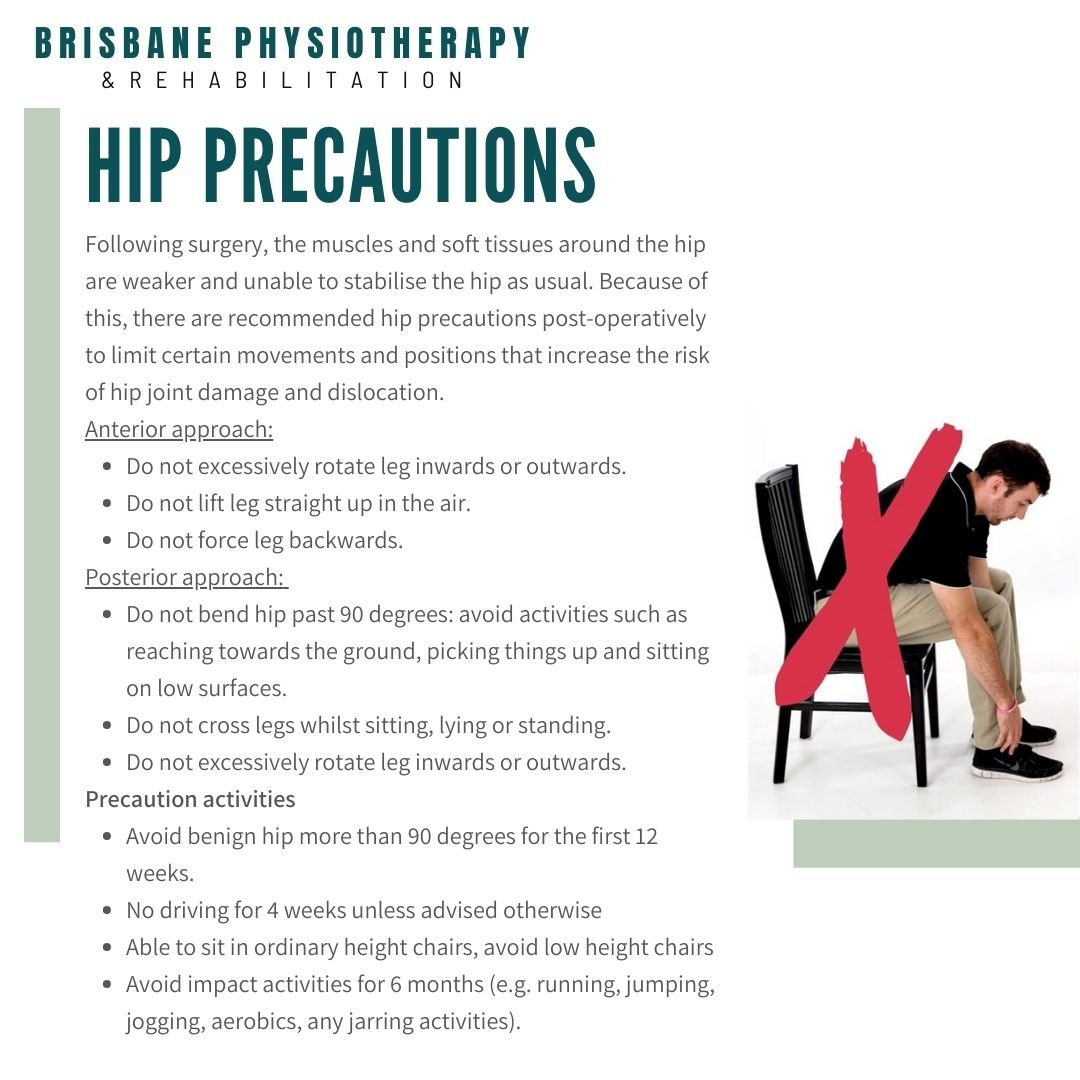
Following surgery, the muscles and soft tissues around the hip are weaker and unable to stabilise the hip as usual. Because of this, there are recommended hip precautions post-operatively to limit certain movements and positions that increase the risk of hip joint damage and dislocation.
- Anterior approach
o Do not excessively rotate leg inwards or outwards.
o Do not lift leg straight up in the air.
o Do not force leg backwards.
- Posterior approach
o Do not bend hip past 90 degrees: avoid activities such as reaching towards the ground, picking things up and sitting on low surfaces.
o Do not cross legs whilst sitting, lying or standing.
o Do not excessively rotate leg inwards or outwards.
Precaution activities:
- Avoid benign hip more than 90 degrees for the first 12 weeks.
- No driving for 4 weeks unless advised otherwise
- Able to sit in ordinary height chairs, avoid low height chairs
- Avoid impact activities for 6 months (e.g. running, jumping, jogging, aerobics, any jarring activities).
Total Hip Replacement Treatment/Rehabilitation
Aim of post-operative rehabilitation: address the functional needs (e.g. start mobilizing) and improve mobility, strength, flexibility and reduce pain. This starts off as an assisted process, but the aim is to get as functional as possible prior to discharge.
Day 0-10:
Circulation and breathing exercises.
Strengthening exercise: hamstring, quadricep inner range, glute bridges.
Range of motion exercises: hip range, standing knee lifts, standing hip abduction, standing hip extension
Functional exercises: quadricep mini lunge, mini squat, standing weight shift.
Hospital Discharge checklist
Able to mobilize safely with mobility aid.
Able to negotiate stairs safely.
Able to get in and out of bed.
Performing exercise program independently
Home services organised to assist with self-cares (if required)
Essential home equipment organised.
Recommended mobility aid purchased/hired (except crutches)
Community Physiotherapy referral organised.
Follow up physiotherapy and home exercise program.
It is recommended to see a private physiotherapist 1 week after discharge from hospital and continue weekly physiotherapy sessions as guided by the physiotherapist and your surgeon.
Physiotherapy will assist in progressing your mobility off crutches and progressing exercises to strengthen and restore range of motion and flexibility to the hip.