What Is Lumbar Foraminal Stenosis?
Lumbar Foraminal Stenosis
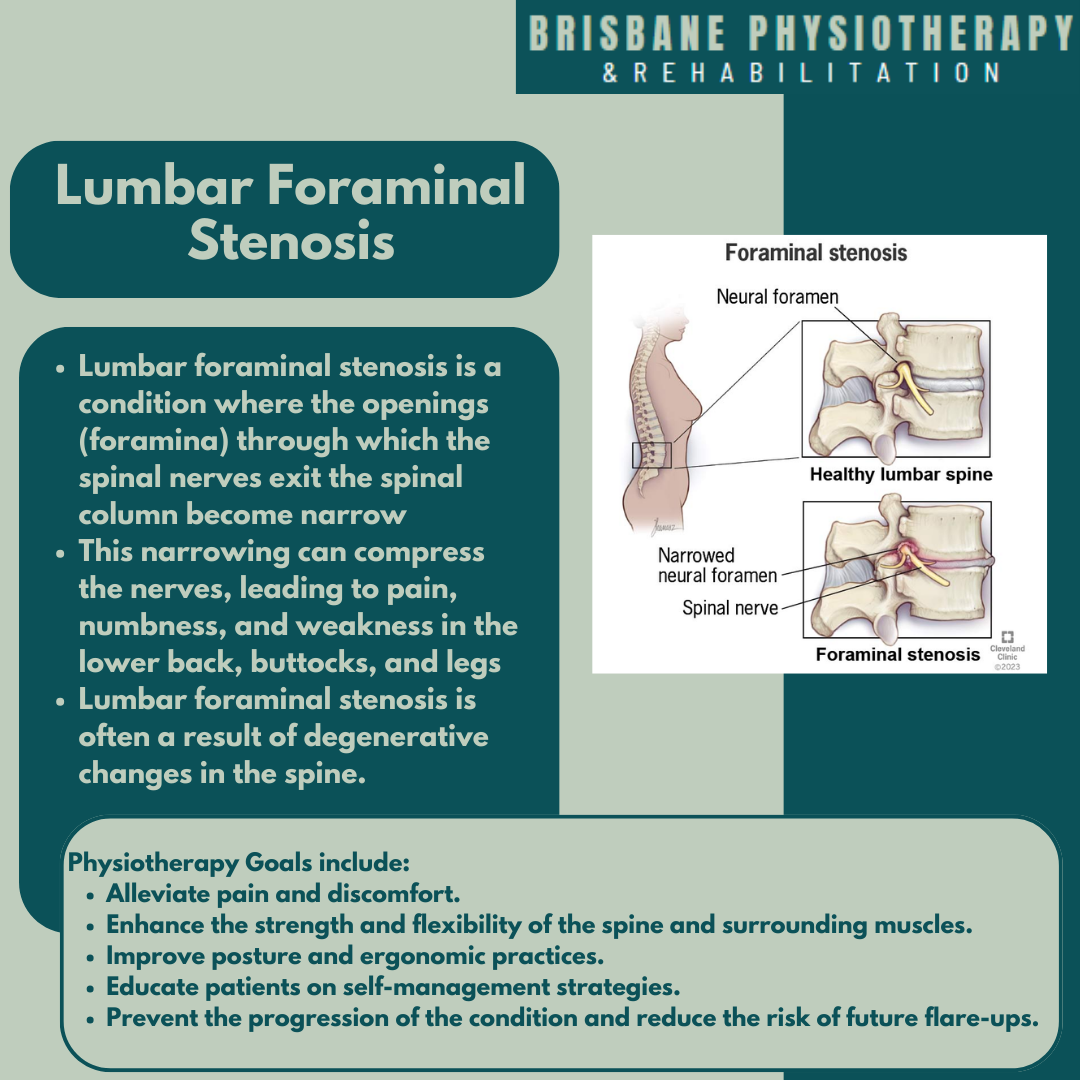
Lumbar foraminal stenosis is a condition where the openings (foramina) through which the spinal nerves exit the spinal column become narrowed. This narrowing can compress the nerves, leading to pain, numbness, and weakness in the lower back, buttocks, and legs. Lumbar foraminal stenosis is often a result of degenerative changes in the spine.
Symptoms of Lumbar Foraminal Stenosis
The symptoms of lumbar foraminal stenosis can vary depending on the severity and specific nerves affected. Common symptoms include:
Lower Back Pain: Persistent or intermittent pain in the lower back.
Radiculopathy: Pain that radiates from the lower back to the buttocks, thighs, and legs, often described as sharp, burning, or shooting pain.
Numbness and Tingling: Sensations of pins and needles or numbness in the legs and feet.
Weakness: Muscle weakness in the legs, which can affect walking and balance.
Sciatica: Pain along the sciatic nerve pathway, typically on one side of the body.
Reduced Reflexes: Diminished reflex responses in the lower extremities.
Causes of Lumbar Foraminal Stenosis
Several factors can contribute to the development of lumbar foraminal stenosis, including:
Degenerative Disc Disease: As discs lose height and hydration, they can bulge and reduce the space in the foramina.
Osteoarthritis: Wear and tear of the spinal joints can lead to bone spur formation, which narrows the foramina.
Thickened Ligaments: Ligaments in the spine can become thickened and stiffen with age, encroaching on the foramina.
Herniated Discs: Protruding discs can press on the nerves exiting the spine.
Spondylolisthesis: A condition where one vertebra slips forward over the one below it, narrowing the foramina.
Physiotherapy Management for Lumbar Foraminal Stenosis
Physiotherapy is a key component of managing lumbar foraminal stenosis, focusing on relieving symptoms, improving function, and enhancing the quality of life. Treatment is typically tailored to the individual's specific symptoms and needs.
Exercise Therapy
Strengthening Exercises: Targeting the core, back, and leg muscles to provide better support for the spine and improve stability.
Flexibility Exercises: Stretching exercises to improve flexibility in the lumbar spine and lower extremities, reducing stiffness.
Aerobic Exercises: Low-impact activities such as walking, swimming, or cycling to improve overall cardiovascular health and aid in weight management.
Manual Therapy
Mobilisation: Gentle techniques to improve joint mobility and reduce stiffness in the lumbar spine.
Soft Tissue Massage: To relax tight muscles, improve circulation, and reduce pain.
Postural Training
Posture Correction: Training on proper posture to reduce strain on the lower back.
Ergonomic Advice: Recommendations for optimal workstation setup and proper body mechanics during daily activities.
Functional Training
Gait Training: Exercises and techniques to improve walking patterns and reduce discomfort during movement.
Activity Modification: Strategies to modify daily activities to minimize pain and prevent exacerbation of symptoms.
Education and Self-Management
Home Exercise Programs: Tailored exercises to be performed regularly at home.
Lifestyle Modifications: Advice on maintaining a healthy weight, staying active, and avoiding activities that worsen symptoms.
Physiotherapy Goals
The primary goals of physiotherapy for lumbar foraminal stenosis are to:
Alleviate pain and discomfort.
Enhance the strength and flexibility of the spine and surrounding muscles.
Improve posture and ergonomic practices.
Educate patients on self-management strategies.
Prevent the progression of the condition and reduce the risk of future flare-ups.
By addressing both the symptoms and underlying causes of lumbar foraminal stenosis, physiotherapy can significantly improve a patient's quality of life, enabling them to manage their condition effectively and maintain their independence. Regular follow-ups and adjustments to the treatment plan ensure ongoing management and optimal outcomes.