Frozen Shoulder
What is Frozen Shoulder?
Adhesive capsulitis, commonly known as frozen shoulder, is a painful and debilitating condition characterized by pain, shoulder stiffness and limited shoulder mobility. This condition can significantly impact daily activities and quality of life. To effectively manage frozen shoulder, it's essential to understand its anatomy and how it develops.
Anatomy of Frozen Shoulder:
Frozen shoulder primarily affects the glenohumeral joint, where the upper arm bone (humerus) meets the shoulder blade (scapula). Key components include:
Shoulder Joint Capsule: A flexible yet tough connective tissue that surrounds the shoulder joint, keeping it stable.
Synovial Fluid: A lubricating fluid within the joint capsule that facilitates smooth shoulder movement.
Development of Frozen Shoulder:
Frozen shoulder typically progresses through three stages:
Freezing Stage: In this stage, patients experience increasing shoulder pain and a gradual loss of motion. The shoulder joint capsule thickens and tightens, leading to pain and stiffness.
Frozen Stage: Pain may begin to diminish, but severe shoulder stiffness becomes more pronounced. Movements are significantly limited.
Thawing Stage: Gradually, the shoulder begins to regain motion. This stage can take several months to years.
Common Risk Factors of Frozen Shoulder:
Several factors may increase the risk of developing frozen shoulder:
Age: It is more common in individuals over 40, with the risk increasing with age.
Gender: Women are more likely to develop frozen shoulder.
Certain Health Conditions: Conditions like diabetes, heart disease, and thyroid disorders are associated with an increased risk.
Shoulder Trauma or Surgery: Injuries or surgeries involving the shoulder can trigger the condition.
Signs and Symptoms of Frozen Shoulder:
Common signs and symptoms of frozen shoulder include:
Pain: Often a dull or aching pain in the shoulder that worsens with movement.
Stiffness: Gradual loss of shoulder mobility, limiting range of motion.
Difficulty Sleeping: Pain and stiffness can make it challenging to sleep on the affected side.
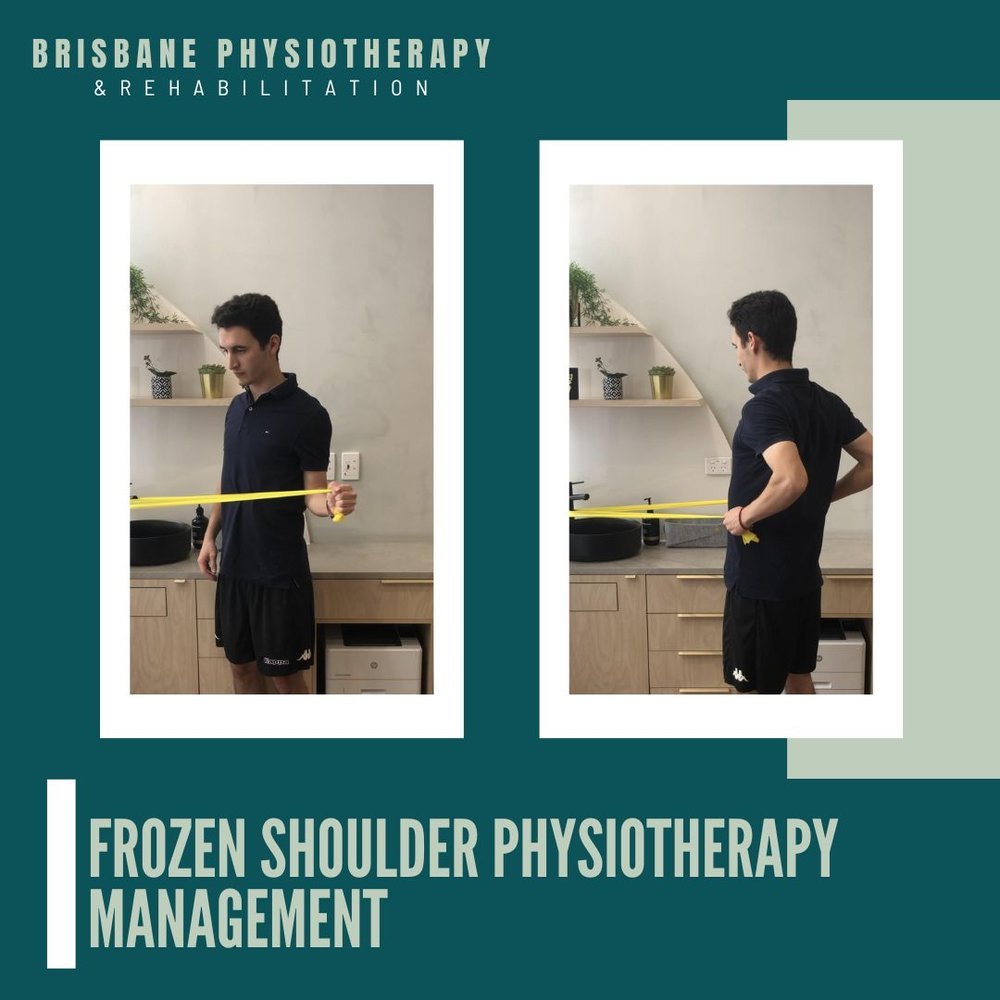
Frozen Shoulder Physiotherapy Management
Managing frozen shoulder involves a multi-faceted approach to alleviate pain, improve shoulder function, and restore quality of life. Understanding these strategies is key to effectively managing this challenging condition.
Frozen Shoulder Management Strategies:
Pain Management:
Medications: Over-the-counter pain relievers like ibuprofen or prescribed medications may be used to manage pain and inflammation. Always follow dosage instructions and consult your healthcare provider before starting any medication.
Physical Therapy:
Range of Motion Exercises: A physical therapist will guide you through a series of gentle exercises to gradually regain shoulder mobility. These exercises are tailored to your specific condition and may be performed regularly.
Stretching: Stretching exercises target the tight shoulder capsule and surrounding tissues to improve flexibility.
Strengthening: Strengthening exercises focus on the muscles around the shoulder joint to enhance stability and support.
Heat and Cold Therapy:
Heat Application: Applying heat to the shoulder before exercise or stretching can help relax tight tissues and reduce stiffness.
Cold Compress: Cold therapy may be used to reduce inflammation and alleviate pain after physical therapy or exercises.
Corticosteroid Injections:
In some cases, a healthcare provider may recommend corticosteroid injections into the shoulder joint to reduce inflammation and pain.
Hydrodilatation:
This procedure involves injecting sterile water into the shoulder joint to stretch the capsule and improve mobility. It is usually performed under ultrasound guidance.
Home Exercises:
Performing prescribed exercises at home is essential to maintain progress made during physical therapy sessions.
Activity Modification:
Modify or avoid activities that exacerbate symptoms or place excessive strain on the shoulder.
Patient Education:
Understanding the condition, its stages, and the importance of adherence to prescribed exercises and treatments is crucial for successful management.
Lifestyle Modifications:
Pay attention to posture and ergonomics in daily activities to minimize stress on the shoulder.
Gentle, regular stretching exercises can help maintain shoulder mobility and prevent recurrence.